New implantable sensor may allow long-term monitoring of cancer cells and glucose
Carbon nanotubes that detect nitric oxide can be implanted under the skin for more than a year
November 4, 2013

Carbon nanotubes are encapsulated within a hydrogel, allowing them to be implanted under the skin (credit: Bryce Vickmark)
Nitric oxide (NO) is one of the most important signaling molecules in living cells, carrying messages within the brain and coordinating immune system functions. In many cancerous cells, levels are perturbed.
“Nitric oxide has contradictory roles in cancer progression, and we need new tools in order to better understand it,” says Michael Strano, the Carbon P. Dubbs Professor of Chemical Engineering at MIT. “Our work provides a new tool for measuring this important molecule, and potentially others, in the body itself and in real time.”
The sensors can be implanted under the skin and used to monitor inflammation — a process that produces NO. This is the first demonstration that nanosensors could be used within the body for this extended period of time.
Such sensors could also be adapted to detect other molecules, including glucose. Strano’s team is now working on sensors that could be implanted under the skin of diabetic patients to monitor their glucose or insulin levels, eliminating the need to take blood samples.
Sensors for variety of molecules
Strano’s lab has recently developed carbon nanotube sensors for a variety of molecules, including hydrogen peroxide and toxic agents such as the nerve gas sarin. Such sensors take advantage of carbon nanotubes’ natural fluorescence, by coupling them to a molecule that binds to a specific target. When the target is bound, the tubes’ fluorescence brightens or dims.
Strano’s lab has previously shown that carbon nanotubes can detect NO if the tubes are wrapped in DNA with a particular sequence. In a new paper in Nature Nanotechnology , the researchers modified the nanotubes to create two different types of sensors: one that can be injected into the bloodstream for short-term monitoring, and another that is embedded in a gel so it can be implanted long-term under the skin.
To make the particles injectable, postdoc Nicole Iverson attached PEG, a biocompatible polymer that inhibits particle-clumping in the bloodstream. She found that when injected into mice, the particles can flow through the lungs and heart without causing any damage. Most of the particles accumulate in the liver, where they can be used to monitor NO associated with inflammation.
“So far we have only looked at the liver, but we do see that it stays in the bloodstream and goes to kidneys. Potentially we could study all different areas of the body with this injectable nanoparticle,” Iverson says.
The longer-term sensor consists of nanotubes embedded in a gel made from alginate, a polymer found in algae. Once this gel is implanted under the skin of the mice, it stays in place and remains functional for 400 days; the researchers believe it could last even longer. This kind of sensor could be used to monitor cancer or other inflammatory diseases, or to detect immune reactions in patients with artificial hips or other implanted devices, according to the researchers.
Once the sensors are in the body, the researchers shine a near-infrared laser on them, producing a near-infrared fluorescent signal that can be read using an instrument that can tell the difference between nanotubes and other background fluorescence.
The research was funded by a grant from Sanofi-Aventis, and also partly by the National Institutes of Health, the National Cancer Institute, the National Institute of Environmental Health Sciences, a Beckman Young Investigator Award, and the National Science Foundation.
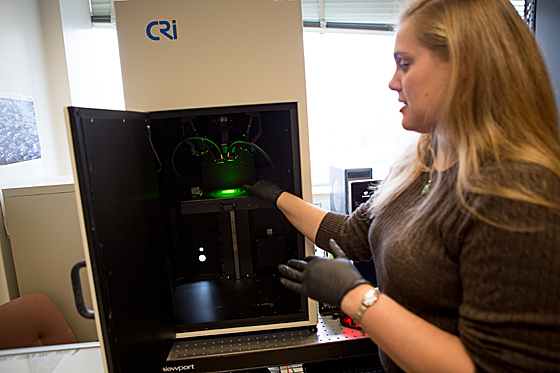
Postdoc
Nicole Iverson demonstrates the instrument used to measure the
fluorescent signal from nanotube sensors that detect nitric oxide
(credit: Bryce Vickmark)
Iverson is now working on adapting the technology to detect glucose, by wrapping different kinds of molecules around the nanotubes.
Most diabetic patients must prick their fingers several times a day to take blood glucose readings. While there are electrochemical glucose sensors available that can be attached to the skin, those sensors last only a week at most, and there is a risk of infection because the electrode pierces the skin.
Furthermore, Strano says, the electrochemical sensor technology is not accurate enough to be incorporated into the kind of closed-loop monitoring system that scientists are now working toward. This type of system would consist of a sensor that offers real-time glucose monitoring, connected to an insulin pump that would deliver insulin when needed, with no need for finger pricking or insulin injection by the patient.
“The current thinking is that every part of the closed-loop system is in place except for an accurate and stable sensor. There is considerable opportunity to improve upon devices that are now on the market so that a complete system can be realized,” Strano says.
Abstract of Nature Nanotechnology paper
Single-walled carbon nanotubes are particularly attractive for biomedical applications, because they exhibit a fluorescent signal in a spectral region where there is minimal interference from biological media. Although single-walled carbon nanotubes have been used as highly sensitive detectors for various compounds, their use as in vivo biomarkers requires the simultaneous optimization of various parameters, including biocompatibility, molecular recognition, high fluorescence quantum efficiency and signal transduction. Here we show that a polyethylene glycol ligated copolymer stabilizes near-infrared-fluorescent single-walled carbon nanotubes sensors in solution, enabling intravenous injection into mice and the selective detection of local nitric oxide concentration with a detection limit of 1 µM. The half-life for liver retention is 4 h, with sensors clearing the lungs within 2 h after injection, thus avoiding a dominant route of in vivo nanotoxicology. After localization within the liver, it is possible to follow the transient inflammation using nitric oxide as a marker and signalling molecule. To this end, we also report a spatial-spectral imaging algorithm to deconvolute fluorescence intensity and spatial information from measurements. Finally, we demonstrate that alginate-encapsulated single-walled carbon nanotubes can function as implantable inflammation sensors for nitric oxide detection, with no intrinsic immune reactivity or other adverse response for more than 400 days.
(¯`*• Global Source and/or more resources at http://goo.gl/zvSV7 │ www.Future-Observatory.blogspot.com and on LinkeIn Group's "Becoming Aware of the Futures" at http://goo.gl/8qKBbK │ @SciCzar │ Point of Contact: www.linkedin.com/in/AndresAgostini
 Washington
Washington